BPC-157 vs TB-500: Research Peptide Comparison Guide
Share
BPC-157 promotes localized healing, angiogenesis, and gut repair, making it ideal for tendon and ligament studies. TB-500 supports systemic recovery by enhancing cell migration and actin regulation, making it better suited for muscle regeneration and widespread tissue repair models.
Both peptides are widely used in preclinical research, but their mechanisms, applications, and outcomes are fundamentally different. Choosing the right one depends on whether your focus is localized versus systemic repair, neuroinflammation versus muscle remodeling, or tendon versus vascular tissue models.
This comparison draws attention from a wide range of professionals and curious minds. Biohackers often explore these peptides for accelerated recovery and tissue resilience. Researchers rely on them to study wound healing, gut integrity, and systemic inflammation in vitro.
Athletes and coaches examine their potential in soft tissue regeneration, while wellness-focused clinics look to the literature for compliant research applications. Even science-first hobbyists are diving deep, fascinated by how angiogenesis, cytoprotection, and cellular repair may be modulated at the molecular level.

If you're looking for a side-by-side breakdown of BPC-157 and TB-500, how they work, where they shine, and what makes them different, read on.
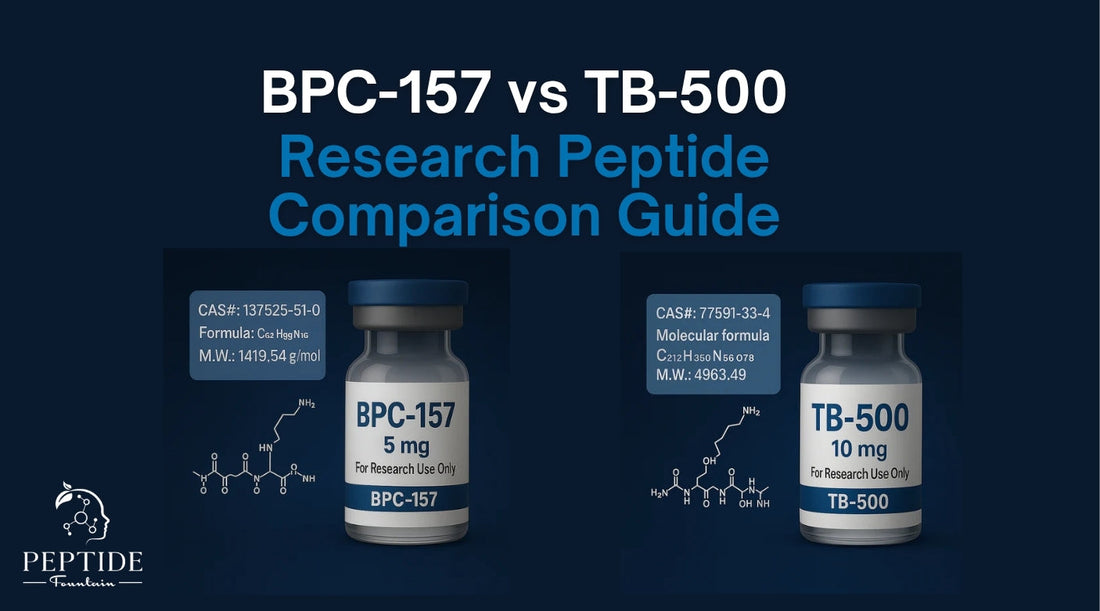
Origin and Molecular Profile
Both BPC-157 and TB-500 fall under the category of synthetic peptides used in laboratory research, yet they originate from very different biological templates.
BPC-157 is a synthetic fragment derived from a naturally occurring protein found in human gastric juice, specifically, a pentadecapeptide composed of 15 amino acids. This fragment has been shown in research models to play a role in angiogenesis, collagen synthesis, and GI mucosal integrity, making it a compound of interest in studies related to tendon repair and gut-brain interactions.
TB-500, by contrast, is a synthetic version of thymosin beta-4, a 43-amino acid protein found ubiquitously in animal cells. TB-500 is not a direct analog but rather a short, bioactive peptide sequence designed to mimic the regenerative effects of thymosin beta-4. Its most well-known function involves actin binding, a process vital to cell migration, tissue remodeling, and wound healing in systemic models.
Structural and Functional Differences
Structurally, the two peptides differ in size, composition, and pharmacokinetic behavior.
BPC-157 is smaller and more focused in its tissue targets, often demonstrating stability even in the presence of gastric enzymes, prompting interest in its oral bioavailability under specific lab conditions.
TB-500, on the other hand, is designed for systemic circulation, typically administered through injection and evaluated for its impact on large-scale tissue regeneration and muscular endurance.
Functionally, the peptides operate via distinct biological pathways. BPC-157 appears to regulate nitric oxide (NO) pathways, a mechanism implicated in vascular repair, inflammation control, and neuroprotection. TB-500 exerts its effects by binding to actin, promoting cytoskeletal reorganization, a key process in cellular migration and tissue regeneration.
Therefore, BPC-157 focuses on localized repair, particularly in poorly vascularized tissues like tendons and ligaments, while TB-500 drives systemic healing through widespread cellular activation and migration. These foundational differences is key to determining which peptide aligns with a given research model.
How They Work
BPC-157 Pathways
BPC-157 demonstrates its effects primarily through localized mechanisms that support tissue repair, vascular growth, and gastrointestinal stability. One of its central pathways involves the stimulation of angiogenesis, facilitated by upregulation of VEGF (vascular endothelial growth factor) and FGF (fibroblast growth factor). This process is vital in healing tissues with limited blood supply, such as ligaments and tendons.
In gastrointestinal models, BPC-157 has shown a protective effect on the mucosal lining, making it a compound of interest in studies involving ulcers, intestinal permeability, and inflammatory conditions of the gut. Its origin from a gastric protein fragment may contribute to this targeted action.
Additionally, BPC-157 is thought to modulate nitric oxide (NO) signaling, a pathway linked to both vascular health and neuroinflammation. This interaction supports collagen synthesis and may contribute to neuroprotective effects in research settings focused on nerve regeneration or oxidative stress.
TB-500 Pathways
TB-500 works through a broader, systemic mechanism centered on actin upregulation. Actin is a structural protein essential for cell movement and repair. By enhancing actin dynamics, TB-500 facilitates cellular migration, allowing regenerative cells to travel more efficiently to damaged sites.
This action also appears to promote stem cell mobilization, which contributes to tissue flexibility and structural restoration across various organ systems. In research models, TB-500 has been evaluated for its impact on dermal repair, muscle recovery, and even cardiovascular tissue remodeling.
Another defining characteristic of TB-500 is its role in systemic inflammation modulation. Rather than targeting a specific localized process, it appears to regulate inflammatory cytokines across the body, making it useful in research exploring full-body injury or multi-tissue repair scenarios.
Together, these peptides demonstrate distinct yet complementary modes of action, BPC-157 focuses on precision healing in vascular, connective, and neural tissues, while TB-500 activates broader mechanisms tied to cellular mobility, elasticity, and immune modulation.
Applications in Research Models
BPC-157 in the Lab
BPC-157 is frequently studied in models involving tendon injuries, gut lining damage, and neuroinflammatory conditions. Its effectiveness in angiogenesis and nitric oxide modulation makes it particularly well-suited for tissue-specific research, especially in poorly vascularized areas like ligaments and connective tissue.
In gastrointestinal models, BPC-157 has demonstrated protective effects on mucosal lining and intestinal permeability, with implications for studies focused on leaky gut, ulcers, and systemic inflammation linked to GI dysfunction. Its localized influence, especially in neuroregeneration and microvascular repair, allows researchers to evaluate its targeted effects in controlled environments.
Most commonly, BPC-157 is administered via subcutaneous injection near the site of injury in preclinical models. This localized delivery method supports its tissue-specific action, allowing researchers to isolate effects in tendon, nerve, or vascular assays with minimal systemic influence.
TB-500 in Experimental Contexts
TB-500, in contrast, is commonly explored in systemic models of trauma, inflammation, and tissue degradation. Its ability to modulate actin and promote stem cell migration makes it relevant in full-body repair models, including those focused on cardiovascular tissue, dermal healing, and skeletal muscle regeneration.
Preclinical studies have highlighted TB-500’s potential in enhancing cardiac remodeling post-injury, accelerating skin wound closure, and restoring muscular integrity after strain or damage. Its systemic scope makes it a compelling candidate for scenarios where multiple tissue types or large injury zones are involved.
Some researchers evaluate TB-500 alongside BPC-157, or in combination with other peptides such as the Wolverine blend, to simulate multi-pathway repair. Whether this stacking offers true synergy or redundancy depends on the specific goals of the experiment. In studies aiming to target both systemic and localized healing simultaneously, this combination may yield complementary benefits without overlapping mechanisms. However, in strictly localized models, such stacking could be unnecessary.
Comparison Table: BPC-157 vs TB-500
When selecting between BPC-157 and TB-500 for research purposes, you need to know their core differences. Below is a side-by-side breakdown of key features to help guide experimental design and compound selection:
|
Feature |
BPC-157 |
TB-500 |
|
Origin |
Human gastric protein |
Synthetic Thymosin Beta-4 analog |
|
Mechanism |
Angiogenesis + nitric oxide modulation |
Actin remodeling + cell migration |
|
Strengths |
Tendons, GI tract, neuroprotection |
Muscles, skin, systemic inflammation |
|
Administration |
Oral or injectable |
Injectable only |
|
Best Use Cases |
Targeted repair |
Broad tissue regeneration |
|
Injection Preference |
Localized |
Systemic |
This comparison underscores how each peptide serves a distinct research purpose: BPC-157 excels in highly localized, tissue-specific models, while TB-500’s broader systemic activity is better suited for full-body regeneration studies. Selecting the right peptide, or using them in complementary tandem, depends entirely on the scope and intent of your study.
Protocol Considerations and Stability
Storage and Shelf Life
Proper storage and handling are critical to preserving the integrity of both BPC-157 and TB-500 in a research setting. For long-term storage, -20°C is recommended to maintain molecular stability and prevent degradation.
Once reconstituted, typically with bacteriostatic water, both peptides remain stable for approximately 2 to 4 weeks when refrigerated between 2–8°C. BPC-157, in particular, has been observed to maintain structural stability within this window under standard lab conditions, though exact duration may vary based on environmental factors like temperature fluctuations and storage vial quality.
Reconstitution & Handling
For reconstitution, bacteriostatic water remains the preferred solvent due to its preservative qualities and compatibility with most peptide structures. DMSO and other solvents should only be used if explicitly validated for the experiment at hand, as they may compromise peptide stability or introduce unwanted variables.
When preparing either peptide, avoid vigorous shaking or rapid agitation, gentle swirling is sufficient. Aggressive mixing can damage the peptide’s structure, reducing its activity in vitro.
Additionally, light sensitivity is a concern, especially with TB-500. To prevent degradation from UV exposure, it's best to store reconstituted solutions in amber-colored vials or in a dark environment, further ensuring the consistency and reliability of experimental outcomes.
By following these basic but critical guidelines, researchers can minimize degradation risks and ensure that their peptides maintain full potency throughout their intended research use.
Can They Be Used Together?

Synergy in Research Models
In certain research settings, combining BPC-157 and TB-500 may provide additive or even synergistic effects. Because these peptides operate through distinct biological pathways, BPC-157 via angiogenesis and nitric oxide modulation, and TB-500 through actin-driven cellular migration, their combined use can support multi-tissue recovery models.
For example, in simulations involving ligament injuries alongside muscular or gastrointestinal trauma, using both peptides may enhance outcomes by addressing both localized repair and systemic regeneration.
Researchers exploring complex injury cascades, such as post-surgical recovery or full-body inflammatory conditions, often find this dual approach beneficial for accelerating wound closure, supporting multi-layered tissue repair, and suppressing widespread inflammation.
When to Avoid Combining
However, co-administration is not always necessary. In tightly focused studies, such as those involving isolated tendon lesions or single-organ injury models, stacking both peptides could introduce unnecessary variables or dilute the ability to isolate one compound’s effect.
In these cases, using a single, well-matched peptide often leads to cleaner data and a more defined understanding of outcomes.
As always, the decision to combine should be driven by research design. When evaluating systemic versus localized recovery dynamics, knowledge of each peptide’s mechanism and target scope is needed for generating meaningful, reproducible data.
Safety, Legality, and Research Use Only
Regulatory Classification
Both BPC-157 and TB-500 are classified as research-only compounds and remain unscheduled in many jurisdictions. This means they are not approved for human or veterinary use, and no claims can be made regarding their therapeutic effects or outcomes outside of controlled scientific environments. Their distribution and usage must remain within the boundaries of lawful laboratory research.
Researchers should source peptides from suppliers who comply with regulatory standards and also provide full transparency on product identity and purity. At Peptide Fountain, every compound is backed by third-party Certificates of Analysis (COAs), batch tracking, and documented sourcing protocols. This level of documentation is vital for ensuring that peptides used in scientific models meet the required standards for purity, potency, and compliance.
Unfortunately, inconsistencies in labeling, unstable formulations, or undisclosed additives are still a concern in the research chemical space. To maintain integrity and reliability in your studies, always verify your source's COA access, batch number, and whether independent testing has been conducted.
By adhering to these practices, researchers remain compliant with the law and also uphold the scientific rigor necessary for valid, reproducible experimentation.
What’s Right for Your Lab?
Choosing between BPC-157 and TB-500 depends entirely on the scope and specificity of your research model. If your work focuses on tendon repair, gastrointestinal injury, or localized neuroregeneration, BPC-157 may offer more targeted, tissue-specific results. Its mechanisms of angiogenesis and nitric oxide modulation make it ideal for precision-driven assays and microvascular recovery studies.
TB-500, in contrast, lends itself well to systemic injury models, actin-regulated cellular migration, and muscle regeneration protocols. Its broad tissue impact and role in stem cell mobilization allow for more comprehensive modeling of full-body trauma or multi-tissue healing.
For researchers exploring complex wound closure models, multi-tissue inflammation, or the interaction of local and systemic healing processes, co-administration of both peptides, when justified, may provide a complementary toolset for accelerating recovery and dissecting pathway interactions.
Peptide Fountain is committed to equipping you with the tools needed to ask better scientific questions. Our peptides are COA-backed, third-party tested, and crafted for compliance in research-only settings. If you're designing experiments that require consistency, clarity, and integrity, we’re here to support your next breakthrough.
Explore our catalog of research peptides, engineered for inquiry, built for precision.
Frequently Asked Questions
What’s the shelf life after mixing TB-500?
Once reconstituted with bacteriostatic water, TB-500 can remain stable for approximately 2 to 4 weeks if stored in a refrigerator at 2–8°C. Proper cold-chain management and avoidance of repeated temperature fluctuations are key to preserving peptide integrity.
Can you take these orally?
While BPC-157 has shown some oral stability in preclinical models due to its gastric origin, it’s primarily studied in injectable form for consistency. TB-500, on the other hand, is not considered orally bioavailable and is evaluated exclusively through injectable protocols in laboratory settings.
What’s the best injection protocol for BPC-157 in vitro use?
In preclinical models, BPC-157 is often delivered subcutaneously near the targeted site of tissue injury to isolate its localized effects. However, injection location, volume, and frequency should always be tailored to the experimental design and documented clearly in research protocols.
Can they be used in the same syringe?
While some researchers combine peptides for efficiency, co-mixing in a single syringe is not universally recommended without first verifying solvent compatibility and peptide stability when combined. Always consult available COA and solubility data before co-administering.
Are there solvents that degrade peptide integrity?
Yes. Certain solvents, especially organic solvents like DMSO, can degrade or denature peptides unless validated for the specific compound. For most peptide research, bacteriostatic water is the safest and most compatible option for reconstitution. Proper storage in light-protected, sterile vials is also needed to prevent oxidation and breakdown.


